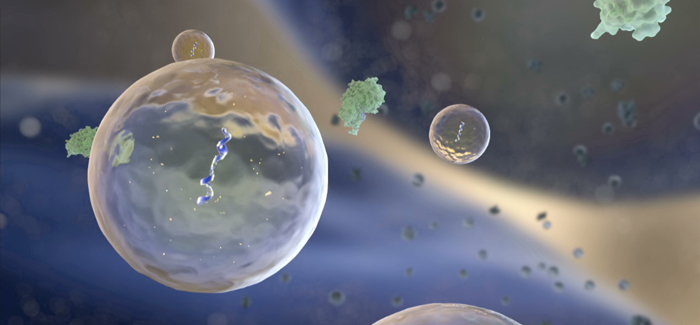
Among their other functions, exosomes ferry microRNA between cells. (National Institutes of Health Common Fund)
UChicago neuroscientists study how “little bubbles” produced by the body’s cells could treat MS.
Research by UChicago neurologists may point the way toward a novel treatment for multiple sclerosis. Building on the long-held scientific belief that a life of physical, intellectual, and social activity helps keep the brain healthy and young, researchers are developing a method to repair, at the cellular level, some of the accumulated wear and tear that afflicts aging brains.
As the brain gets older, it tends to lose myelin, a material that insulates its circuitry and allows neurons to reliably send signals to each other. In people with multiple sclerosis, the immune system wantonly destroys myelin, disrupting the signals between nerve cells and causing severe neurological disability. These symptoms worsen as time goes on and the brain becomes less able to repair the myelin that’s been destroyed.
Current treatments for the disease work by dialing down the immune cells that attack the central nervous system, but they don’t repair the damage that’s been done.
By developing therapies to regenerate myelin UChicago neurobiologist Richard Kraig and Aya Pusic, a graduate student in neurology, are working to help reverse this aspect of the brain’s aging process. One promising line of research explores the effects of keeping an active lifestyle. “Environmental enrichment,” Kraig calls it. He gives an example: taking a walk outside with friends while memorizing your surroundings.
To test the effects of environmental enrichment, Kraig, the William D. Mabie professor in the neurosciences, and Pusic put older rats in a cage with areas to socialize and exercise, including a maze the animals had to navigate to reach their food. “The animals get to climb, run through mazes, run on running wheels,” Kraig says. “We change the complex environment several times a week so they have new mazes to run through.” After this regimen, the rats’ cells began producing a byproduct that encouraged the growth of myelin. When applied to brain slices that had been artificially demyelinated, samples taken from the serum of these older, active rats regenerated myelin just as well as samples taken from young rats, and much better than samples from older rats that hadn’t received the enrichment treatment. These findings were published in February in the journal Glia.
How exactly does a regimen of socializing, learning, and exercising help rebuild myelin? When the rats were exposed to the complex environment, their cells produced small vesicles called exosomes—Pusic calls them “little bubbles.” Many cell types produce exosomes, which carry genetic material and proteins. The exosomes secreted by immune cells during environmental enrichment contain microRNA, a molecule involved in gene expression and regulation. The rats that Kraig and Pusic gave special exercise and socialization produced exosomes containing higher amounts of miR-219, a type of microRNA that encourages stem cells in the brain to develop into cells that make myelin.
To develop their findings into a therapy, the scientists artificially cultured exosomes from rat bone marrow, essentially mimicking the effects of environmental enrichment outside of a living animal. They stimulated the bone marrow cells with a protein important in cell signaling that appears during environmental enrichment. And, just as in the rats, the cells produced exosomes that contained more miR-219.
Kraig says that exosomes could be especially beneficial because they’re all natural. “It is for the first time developing a therapeutic, not from a plant, not from a chemical shelf where various chemicals have been sitting, but this is an intrinsic molecule of a human being, of an animal,” Kraig says. “It’s mimicking Mother Nature’s method of improving myelin.” The production of exosomes is a naturally occurring response, Kraig says, and “that means it’s likely to have a maximal benefit-risk ratio.”
Tests of enriched exosomes have been encouraging: the researchers administered them nasally to older rats and improved their baseline levels of myelin. The next step, Kraig says, is to test enriched exosomes in animals with an impairment that mimics the effect of multiple sclerosis.
Ultimately, the idea is to culture exosomes from the bone marrow of “a healthy relative, or friend, or animal” and introduce them into patients with multiple sclerosis to give their brains a boost of myelin regeneration. This treatment is promising because exosomes “get across the blood-brain barrier easily, and it looks like they’re going specifically to the cells that we need them to go,” Pusic says. The treatment increases myelination without negatively affecting the stem cell pool, which is important for generating more myelin-producing cells.
Kraig and Pusic’s research, funded by a grant from the National Institutes of Health, is on track to start a Phase 1 clinical trial in 2018, which would test the therapy to make sure it’s effective and nontoxic. Kraig is optimistic. “Every other treatment that exists has profound toxic effects,” he says. “If you turn off someone’s immune system, you leave them vulnerable to infections, tumors—bad things.” The researchers believe their treatment has the potential to avoid these risks while repairing the damage done by multiple sclerosis.
Video
Once thought to exist only inside cells, RNA is now known to travel outside of cells and play a role in newly discovered mechanisms of cell-to-cell communication. Are these extracelluar RNAs involved in diseases like cancer, heart disease or neurological diseases like Alzheimer's? Could scientists learn how to use exRNAs to diagnose diseases earlier or even to treat these diseases?
