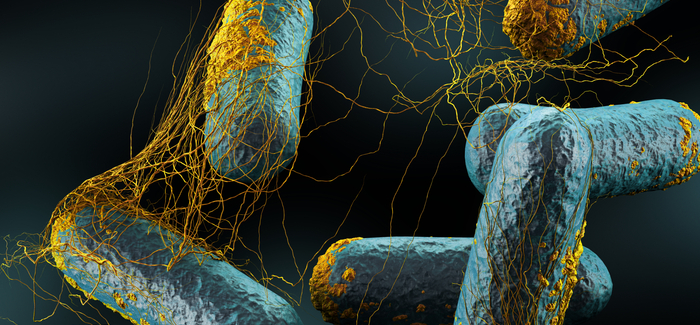
The presence of Clostridia (shown), a common class of gut bacteria, protects against food allergies in mice, according to a new study from Argonne National Laboratory and the University of Chicago Medicine and Biological Sciences. (Image courtesy Argonne, CC BY-NC-SA 2.0)
Exploring the human microbiome.
Right up front, Divinity School Wednesday lunch organizer Terren Wein wanted to remind everyone that “The Microbiome Revolution: Why Microbes Control Your Life!” was not about the Ebola virus. Jack Gilbert, an environmental microbiologist at Argonne National Laboratory and an associate professor in the Department of Ecology and Evolution, didn’t want to scare anybody—or not the way you might think, anyway.
Gilbert explained that we are mostly microbial: for every “human” cell in our bodies—blood cells, bone cells, etc.—there are 10 microbial cells. These 100 trillion microbial cells make up our microbiome, or microbiomes—distinct colonies of microbes in our guts, ears, eyes, mouths, skin, and elsewhere. Every microbiome is unique: because we shed 15 million microbial cells per minute from breathing alone, our overall microbiome is affected by every interaction we’ve had and every place we’ve visited.
That’s not the scary part. In fact, a thriving microbiome does more good than harm.
Gilbert discussed research showing the gut microbiome’s possible role in preventing food allergies, obesity, and even anxiety and depression.
Here’s the scary part. If we destroy large portions of those bacteria, say, through the overuse of antibiotics, the effect can be similar to that of a forest fire: maybe some beneficial effects, some negative effects, and a lot that we just can’t be sure of.
More contact with other microbiomes—human and animal—is probably better for us. But how and why?
Through his work with the American Gut project, Argonne’s Home Microbiome Project, and the Center for Care and Discovery’s Hospital Microbiome Project, Gilbert and other researchers are exploring the complex relationship between people, their microbiomes, and their environments, possibly leading to explanations of the roots of disease and behavior similar to those once promised by the Human Genome Project.
A better understanding of human microbiomes might help treat disorders—physiological and mental—once thought to be hereditary. And it might have more pedestrian uses too. “Maybe you could make a more productive work environment by pumping microbes into the air,” Gilbert said.
The messier and more diverse the microbiome, the better, said Gilbert, who drove to Kentucky with his family to adopt a dog after reading a 2013 study about how dogs might prevent asthma in young children. But he drew a clear distinction between microbes and pathogens.
“Dirty is fine,” he said. “Exposing your kids to the bodily fluids of someone who has Ebola is not fine.”
