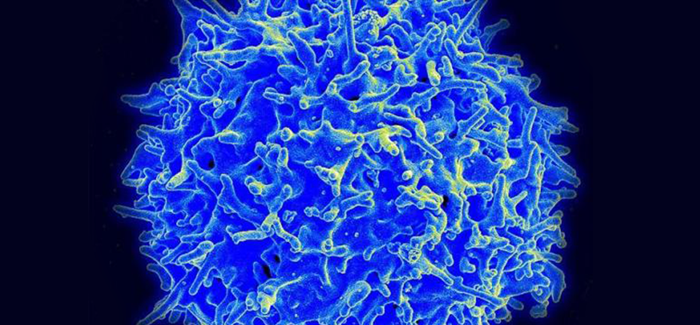
A type of human T cell, a warrior cell is designed to repel invaders. (Image courtesy the National Institute of Allergy and Infectious Disease)
A study of how cancer evades the immune system reveals promising therapeutic potential.
Spontaneous remissions—when a cancer goes away on its own, with no help from medical treatment—are rare. No one quite knows how rare, but estimates range from as high as one in 50,000 to less than one in 100,000 cases, usually for patients with melanoma or kidney cancer.
The lucky patients who have such a remission often attribute their good fortune to divine intervention; clean living; or, less often, to single-malt Scotch. Physicians who witness a case are more likely to credit the immune system. But it makes them wonder: if an immune response can, occasionally, do this on its own, how can we nudge it to do so more often?
In the August 28, 2013, issue of Science Translational Medicine, a team led by Thomas Gajewski, AB’84, PhD’89, MD’91, professor of pathology and medicine at the University of Chicago, provides a closer look at how tumors manage to evade an immune response. Their findings could lead to new therapies—better cancer vaccines, for example—or ways to resensitize tumors and immune cells to each other.
Gajewski and colleagues began by examining a series of human melanomas. When they looked at specific characteristics of the tumor microenvironment, they found two common ways that cancers could dampen or deflect an immune response.
“Some tumors effectively exclude the immune system,” he said. They hide from it or they prevent T cells from invading. Others allow some mingling, an initial dialogue with the immune system, then suppress it. These two categories may require “distinct immunotherapeutic interventions for optimal clinical effect.”
His team focused on tumors that were infiltrated by cytotoxic or CD8+ T cells, warrior cells designed to repel invaders. These patients were more likely to respond, at least initially, to cancer vaccines, yet only a minority of them derived any lasting benefit.
The patients had taken the crucial first step, mounting a targeted immune response against the tumor. So why weren’t the tumors eliminated, or at least held in check? Was the tumor switching off the immune response, or was the immune system learning to tolerate the tumor?
To probe those questions the researchers shifted their attention from human subjects to a series of carefully designed experiments with mice. They found that the immune system, rather than the cancer cells, was behind the peace-making process.
The once-aggressive T cells, having infiltrated the tumors, next proceeded to send out signals that calmed their own initial fury. Tumors that had been infiltrated by aggressive T cells were soon bathed in IDO, an enzyme that contributes to immunologic tolerance; PD-L1, a T-cell inhibitor; and T regulator cells, known as Tregs, that suppress the immune response.
Their finding suggests that PD-L1, IDO, and Tregs could become the next targets for therapy, Gajewski said. Perhaps they could be suppressed by additional immunotherapies, such as anti-PD-1, IDO inhibitors, and Treg-depletion strategies. “Individual tumors have multiple immune suppressive mechanisms,” he said, “so a combined blockade of two or more might be necessary for optimal therapeutic effects.”
“A few years ago, we had no idea that a major subset of patients had a spontaneous immune response against their tumor,” Gajewski said. “We were also surprised to learn that these immune suppressive mechanisms appear to be intrinsic to the host immune system and not directly promoted by the tumor. Knowing this is refining our ability to develop novel therapies.”
