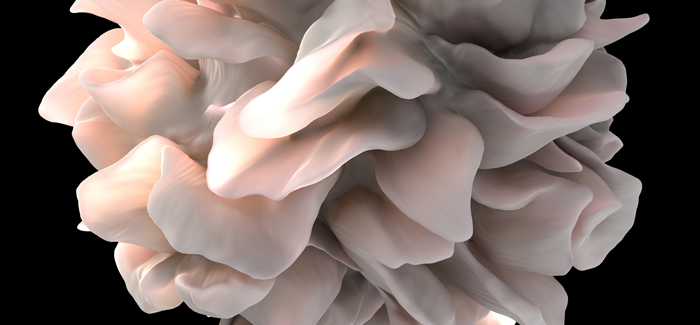
A dendritic cell, which works with T cells to fight tumors. (National Institutes of Health)
Disrupting cancer-cell division, buzz as an economic commodity, surgery that relieves apnea and asthma, and a STING operation to fight disease.
Cancer cell division, disrupted
A new cancer drug developed by UChicago researchers can eradicate human lung cancer cells in mice and shows few side effects. Genetics and cancer researcher Yusuke Nakamura led the study, published October 22 in Science Translational Medicine and coauthored by colleagues Jae-Hyun Park and Houda Alachkar and scientists from a Japanese biopharmaceutical company. The drug destroys cancer cells by disrupting the process of cell division. Says Nakamura: “Everything within the cell spills out; they suffer and die.” In five of six mice, tumors completely disappeared within a month. Coating the drug in liposomes—microscopic bubbles—eliminated its toxicity to the mice’s healthy white and red blood cells.
Buzz feeds the economy
Buzz—the news, gossip, discussion, and excitement surrounding a cultural activity—is not so nebulous a phenomenon as it may seem. According to UChicago sociologist Terry Nichols Clark, buzz is a tradable commodity and political resource and is subject to its own kind of inflation. In Can Tocqueville Karaoke? Global Contrasts of Citizen Participation, the Arts, and Development (Emerald Group Publishing, 2014), the 11th volume in a series on urban policy, Clark, coauthor and series editor, and 18 other scholars analyze civic engagement worldwide and its generative buzz. Among other topics, authors explore how culture and the arts can drive civic participation and economic innovation. The book’s roots trace to Alexis de Tocqueville, who, during his American travels, found that civic groups encouraged democracy. Clark’s research, based in part on a 30-year international survey he coordinates, examines contexts that encourage civic participation and how they vary around the world.
Apnea surgery can ease asthma
Adding strong data to studies suggesting a connection between obstructive sleep apnea and asthma, UChicago researchers found that surgery to treat sleep apnea in children can also ease their asthma. A common pediatric disease, asthma affects an estimated 7.1 million US children under 18 and is the third most frequent cause of hospitalization in those younger than 15. Sleep apnea is also common, affecting 2 to 3 percent of children. In a study of more than 40,000 children between ages 3 and 17, UChicago Medicine researchers Rakesh Bhattacharjee, David Gozal, and Babak Mokhlesi discovered that removing the tonsils and adenoids—a standard therapy for apnea—decreased asthma severity. The surgery reduced acute asthma exacerbations in children by 30 percent, and reduced acute status asthmaticus—a medical emergency—by 38 percent. Asthma-related hospitalizations fell by 36 percent. Coauthored by Beatrix Choi, AB’09, of the UChicago Center for Health and Social Sciences, the study was published in the November PLOS Medicine.
Sting operation fights disease
A newly discovered protein complex in the immune system plays a big role in the body’s ability to detect a tumor and mount a response. Described in a pair of UChicago-based studies, both published November 20 in Immunity, this STING pathway—the acronym stands for Stimulator of Interferon Genes—opens new possibilities in the field of cancer immunotherapy. When the body detects a threat (whether from cancer or infection) marked by damaged or misplaced DNA, a series of chemical reactions activate the STING pathway, which alerts the immune system and helps it identify bad cells and begin to fight them. In one study, led by UChicago pathologist Thomas Gajewski, AB’84, PhD’89, MD’91, researchers identified and illuminated the “stumbling blocks” that sometimes prevent the immune system from destroying cancers. Drugs called “checkpoint inhibitors” can remove the stumbling blocks and take the brakes off the immune response. The other study, led by cancer biologist Yan-Xin Fu and cellular oncologist Ralph Weichselbaum, found that high-dose radiation therapy not only kills tumors but also boosts the body’s natural immune response by damaging cancer cell DNA.
